
Modupe Balogun1, 2* and Emmanuel Ogordi2
1Lagos State University College of Medicine, Ikeja.
2 Department of Ophthalmology, Lagos State University Teaching Hospital, Ikeja Lagos State, Nigeria.
*Corresponding Author: Modupe Balogun, Department of Ophthalmology, Lagos State University Teaching Hospital, Ikeja Lagos State, Nigeria.
Received Date: September 18, 2023
Accepted Date: September 29, 2023
Published Date: October 12, 2023
Citation: Modupe Balogun and Emmanuel Ogordi. (2023) “The Distribution of Refractive Errors in Children Attending a Tertiary Hospital After the Covid-19 Pandemic”, Ophthalmology and Vision Care, 4(1); DOI: 10.61148/2836-2853/JOVC/044.
Copyright: © 2023 Modupe Balogun. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Purpose: To determine a change in the distribution of refractive errors after the COVID-19 pandemic, to proffer solutions to prevent the progression of myopia, and to determine the measures that can be taken for early diagnosis and treatment.
Methods: A retrospective study in which the medical records of all children with refractive errors seen between April 2022 and April 2023 were retrieved. The bio-data of each patient at presentation including the type of refractive error after subjective refraction were extracted from the files.
Results: Five hundred and twenty-four medical records of children with refractive errors between the ages of 5 and 15 years were analyzed.
Introduction:
Refractive error is a vision problem that occurs when the eye cannot focus light accurately on the retina due to the shape of the eye’s components, such as the lens and cornea [1] when the eye is relaxed. This results in blurring vision. Refractive error can be due to an increase or reduction in the axial length of the eye or a change in the curvature of the cornea or the lens. The common types of refraction errors are myopia (near-sightedness), hypermetropia (long-sightedness), astigmatism, and presbyopia which occurs in the elderly.
Uncorrected refractive error is a common cause of visual impairment in the world and also the leading cause of preventable visual impairment, especially in children.
Refractive errors can negatively affect children’s learning, personality development, psychosocial development, and quality of life [2]. If it is not corrected early, it can lead to amblyopia.
It was estimated that 19 million children are visually impaired globally and 12 million of these have uncorrected refractive error (URE) [3].
In a study done in Kazakhstan, it was reported that the overall prevalence of refractive errors in 6-16year old children was 31.6% [4], in Ethiopia, it was 9.4%, [5], while in a study done in Somalia, it was 76.8% in the study participants examined6. Also, in a study done in India, the overall prevalence of refractive errors per 100 children was 8.0 [7], while in Nigeria it was 5.9 % [8]. In December 2019, Coronavirus disease (COVID-19) spread around the world. To prevent the spread, schools were closed down and the authorities had to implement more confinement and introduce e-learning with online classes for school-age children. To prevent the spread of infections, there was a restriction on social gatherings, which led to reduced outdoor activities. The more confinement and e-learning increased the time children were exposed to the digital screen. The digital eye strain among kids (DESK) study 1 reported that the duration of digital device use during the COVID-19 era increased to 3.9±1.9hours compared to 1.9±1.1hours before the COVID-19 era [9]. The restriction to outdoor activities and increased time spent on digital screen time and near-work activities, which are all risk factors for myopia progression stimulated a lot of research. The research showed that 49.8% of the global population will become myopic and 9.8% will have high myopia by 2050 [10]. High myopia can increase the risk of diseases that can cause blindness, such as macular degeneration, retinal detachment, cataract, and glaucoma [11].
Despite the sporadic cases of COVID-19 now and the lifting of the stringent measures put in place to prevent the spread of the disease, children are now observed to use devices like smartphones, computers, and tablets. And, spending more time on the screen exposes them to the modifiable risk factors for myopia.
This study aims to determine if there is a change in the distribution of refractive errors in the study population and to determine the measures that can be taken for early diagnosis and treatment. It also aims to proffer solutions to prevent the progression of myopia and ways to diagnose possible complications early.
Methods: A retrospective study in which the medical records of all children with refractive errors seen between April 2022 and April 2023 were retrieved. The bio-data of each patient at presentation including the type of refractive error after subjective refraction were extracted from the files.
Refractive errors were diagnosed based on best correction with at least +0.50 or -0.50 diopter sphere or diopter cylinder or a combination of both.
Children were grouped according to their age at presentation into the following age groups: children of 5-9 years, preteens of 10-12 years, and teens of 13-15 years. Data were entered and analyzed using the statistical package for social sciences software (SPSS Chicago IL, USA) version 23. Frequency tables were generated for categorical variables. The average table was generated for the scale variable (age), and a test of statistical significance between variables was carried out using the chi-square (x2 ). A p-value of less than 0.05 was accepted as indicative of statistical significance at a 95% confidence level.
Result:
A total of five hundred and twenty-four (524) medical records of children with refractive errors between the ages of 5 and 15 years seen between April 2022 and April 2023 were analyzed.
There were 225(42.9%) males and 299 (57.1%) females seen. The ratio between male and female was 1:1.3.
One hundred and seventy-nine (179) (34.2%) children were within the age range of 5-9 years old. 190 (36.3%) were aged 10-12 years and 155(29.6%) were 13-15 years old. The mean age of the children was 10.5 years old (SD: ±3.0).Table 1.
Distribution of refractive error in the study population showed that myopia occurred in 111(21%) of the children. Amongst this, 14(30%) of the children had high myopia while 97(19%) had simple myopia. Astigmatism was seen in 252 (48%) of the study population. This was further analyzed as simple astigmatism in 86(16.4%) of the population, myopic astigmatism in 81(15.5%), and hyperopic astigmatism in 85(16.2%). Hyperopia was seen in 121(23%) of the children, while anisometropia was recorded in 40(8%) of the study population.Fig.1.
Astigmatism was the most prevalent refractive error, and it was found equally (48% each) in both the male and female children. Further analysis showed that hyperopic astigmatism was more common in male children 48(21.3%).
Hyperopia was seen more in the female children 73(24.4%). Fig. 2.
Total myopia was observed more in the female children 56(18.7%). Further analysis showed high myopia was seen more in the male patients 8(3.6%). Table 2
In 5-9-year-old children, hyperopia occurred in 51(28.5%) of them, while hyperopia astigmatism occurred in 38(21.2%) of them. Myopia and hyperopia were more prevalent in the 10-12-year-old group. Each occurred in 40(21.1%) of the children respectively. For the 13-15-year-old group, myopia was more prevalent in 33(21.3%) of them, while simple astigmatism and myopic astigmatism were seen in 27(17.4%) of the children, respectively.
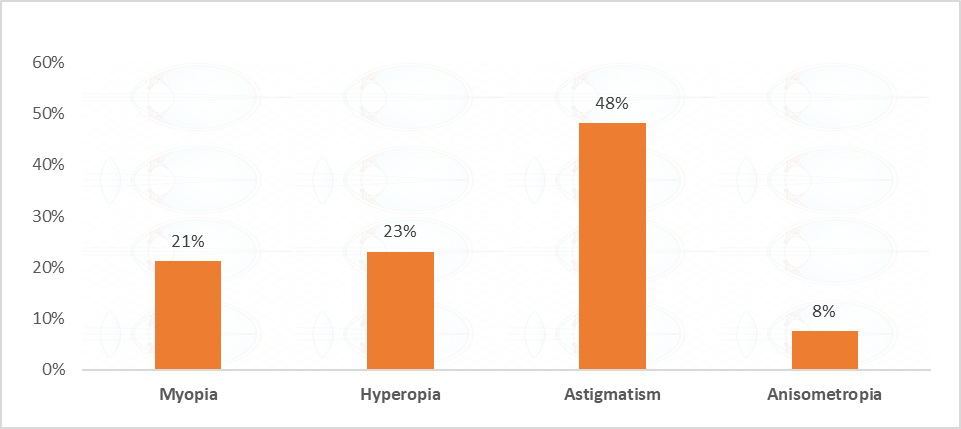
Figure 1: Distribution of Refractive Errors.
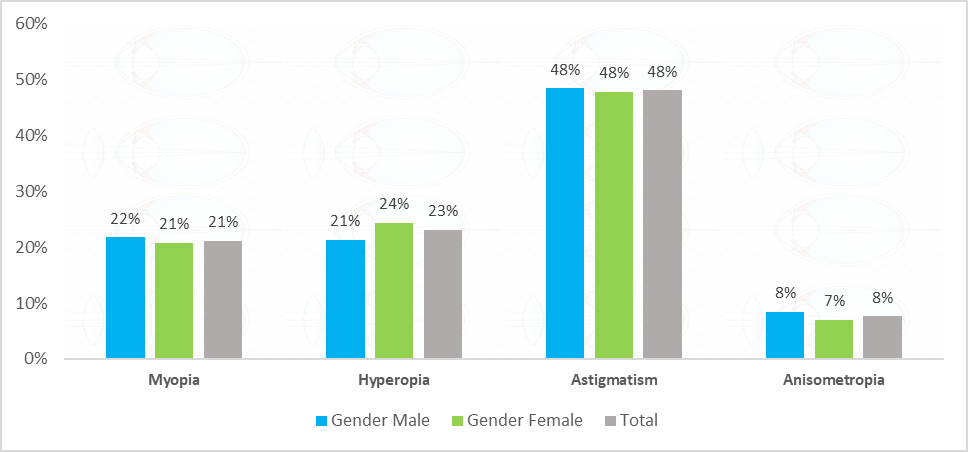
Figure 2: Prevalence of refractive errors among males and females.
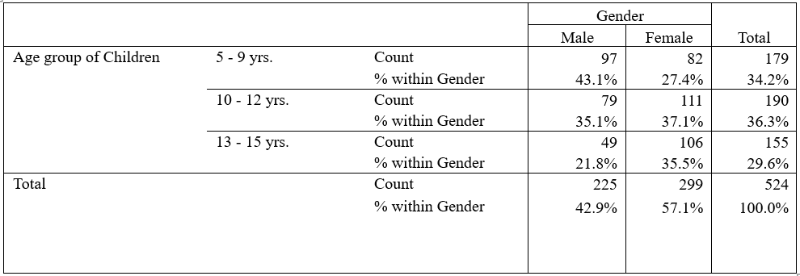
Table1: Age Group of Children and Gender
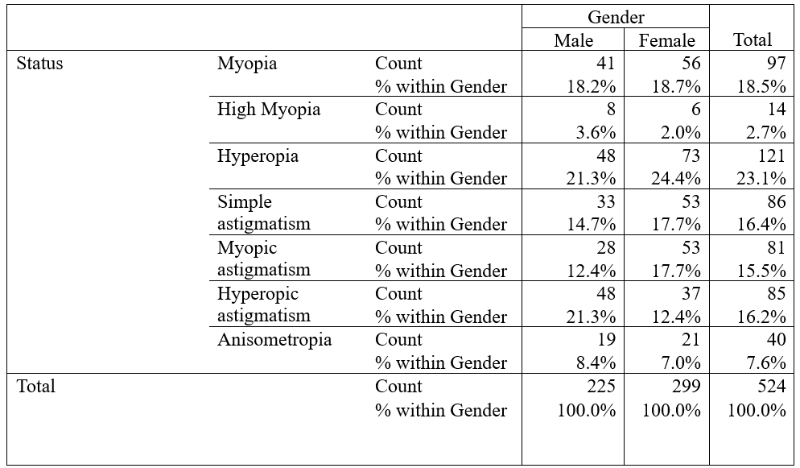
Table 2: Refractive State and Gender.
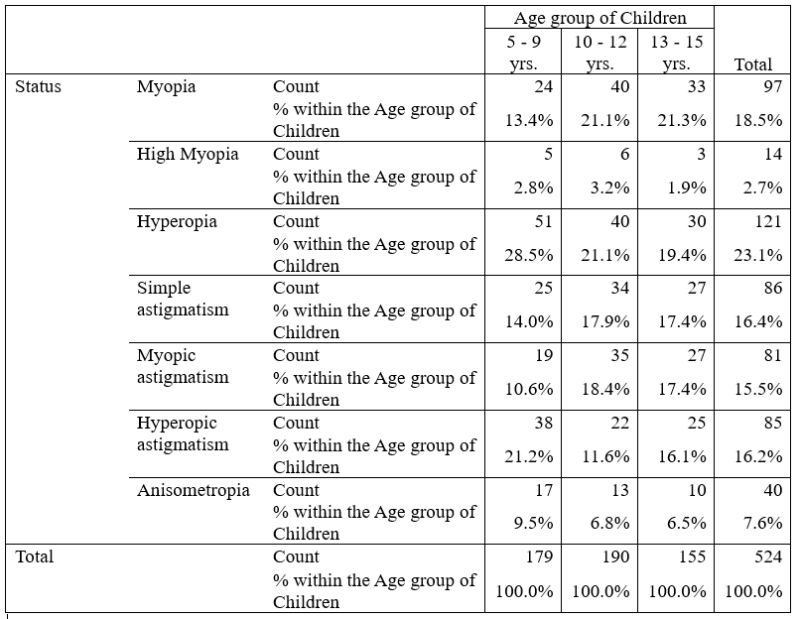 Table 3: Refractive state and Age group of Children
Table 3: Refractive state and Age group of Children
Discussion:
Following the outbreak of the Coronavirus (COVID-19) pandemic that ravaged the world in December 2019, many nations experienced a shutdown of their economies and this affected different sectors and industries globally. The Nigerian educational sector was not left out as schools were closed and many children were engaged in remote learning. Virtual learning interventions and solutions were rolled out, and pioneered by both private and public stakeholders in the educational sector to support the continuation of learning and prevent a learning slide. As a result of remote learning methods, children were exposed to laptops and internet-enabled devices like phones and tablets more than before to aid their learning. This study examines how the COVID-19 pandemic has increased the prevalence of refractive errors among children; identifies the commonest types of refractive errors and proffers possible measures to reduce the progression of the refractive errors.
The medical records of 524 children with refractive errors retrieved showed more female children, 299(1.3:1) had refractive errors. This is similar to a study done by Olusanya et al3, where they recorded a higher number of female children having refractive errors than their male counterparts. The same was also observed by Maduka Okafor et al [12] in their study done on school children, where the prevalence of refractive error was found to be higher in females.
Aditya Sethi [13] and Xiaoyan Yang [14] observed a similar increase in female children with refractive errors in their study. The increase in the prevalence of refractive errors in female children was thought to be because the female hormone peaks earlier than the male hormone during adolescence 14. This area needs more investigation. It could also be probably because girls report to their parents more promptly than males. Contrary to other studies that found refractive errors to be more common in males than in females in their studies. [15,16,17] A study in South Africa found equal distributions of refractive errors between males and females in the study population [18].
The ages of the study population ranged between 5-15 years and the majority were within 10-12 years. Similarly, Olusanya et al, [3] Maduka Okafor et al [12], and Adebisoye et al [8] found the majority of children with refractive errors were older children. Studies done in Ethiopia [5] reported a similar trend. This could be due to increasing visual demand for reading or increased awareness of their visual symptoms at that age. Also, that is the age when they use more devices.
Astigmatism was found to be most prevalent in the study population. It was more in the 13-15-year age group with no gender preference. The astigmatic children had mainly simple astigmatism 86 (16%). This is in line with the findings obtained from a study done in Hong Kong, where 46.5% of the children had astigmatism [19]. Yuan Liang et al [20] recorded a significant increase in astigmatism in the children studied. The difference in the finding is in the age range of the children, who were younger than the study population. This is contrary to a study done that showed fewer cases of astigmatism (0.5%) in children examined after the COVID-19 pandemic [21]. In a similar study done before the COVID-19 pandemic in the same hospital, this study was done on children with refractive errors, astigmatism was also found (42.3%) to be the most common type of refractive error [22]. Simple astigmatism was more common in this present study 86(16%) followed by hyperopic astigmatism 85 (16%) and myopic astigmatism 81(15%).
Hyperopia is thought to be the cause of poor reading habits due to strain in the eyes and asthenopia. In the study population, 121 (23%) were seen to have hyperopia; it was more common in females 73(23%) and 5-9-year-old children. This is in agreement with the study by Yao et al [23] done after COVID-19 where cases of hyperopia were found to be more prevalent in females. This observation is consistent with what was seen in a study done before the COVID-19 pandemic in the same hospital but was seen in the older age group of 8-10 years [22]. This observation is contrary to the study of Trovato et al [24] done in Italy and that of Pratik Sharma et al [25] done in India, in which myopia was found to be more prevalent after the COVID-19 era.
This observation may be difficult to explain because the study location is in an urban area though cosmopolitan with a combination of educated, semi-educated, and non-educated children coming to the same hospital. The fact that hyperopia is more common at lower levels of education and lower educational status cannot be substantiated in this study, though most of the children were from the middle to low-income class.
Myopia was the third common refractive error found in 111-21% of the study population, with simple myopia seen in 97(18.5%) and high myopia in 14(2.7%). This refractive error was more prevalent in the 10-12 years age group. Myopia was on the increase in studies done post-covid 19 era.[6, 17,24]. Fewer studies showed the prevalence of hyperopia after the pandemic but faster progression of myopia though still lower than hyperopia [19]. The early manifestations of myopia in 10-12-year-olds could be a result of the increased time spent on TV and computers, which increased the time spent on near-work activities and reduced the time spent on outdoor activities during the lockdown and after. This is contrary to some studies that found myopia in younger age groups [6, 17, 20] but similar to the pre-COVID period when myopia was noticed more in older age
Group [21].
According to the results of this study, the prevalence of anisometropia was found in 40(8%) of the children and more in males between 5-9 years old. This is contrary to a study, which found anisometropia to be high in the study population (school children) and it was said to increase with older age [26, 27]. A study done in the same study location before COVID-19 observed a similar low prevalence of anisometropia [22], but the age range was older.
Though the short-term period of epidemic isolation seems to have minimal impact on the refractive state of the children studied, precautions need to be taken as most of the children are now inclined to the use of computers, smartphones, and other devices for recreational and, educational purposes. This increases the time they spend on near-work activities and reduces the time spent on outdoor activities. The long-term effect of this is possible myopia and myopia progression as previously healthy children can develop myopia and there would be faster progression of myopia in those who already have it. There could be a rise in the incidence of high myopia associated with a high risk of vision-threatening pathologies such as Glaucoma, Retinal detachment, macular degeneration, and cataract [11]. It was estimated that by the year 2050, 5 million people worldwide will be myopic [10] due to the shaping of the long-term changes, which is conducive to the onset and progression of myopia. Though some studies found that time spent on screen is not associated with the prevalence of myopia [28], other studies found an association between computer use and myopia [29]. Given this, policies have to be put in place by the government, schools, and parents.
The following recommendations should be considered. Government should create awareness by educating the public on the effect of reduced outdoor time on the incidence and progression of myopia.
School health initiatives should be a part of the national eye health program and teachers should be trained to perform vision screening in schools periodically. Eye examination should be enforced before school enrollment for early detection and treatment of eye diseases in children and the government should ensure treatment is available and affordable for children.
Schools should consider going back to the traditional way of teaching (in the classroom) and reducing the use of electronics as a teaching tool.
Schools should incorporate outdoor activities into school time to encourage students to rest their eyes.
At home, parents should monitor the time their children spend on screen and reduce their use of phones, tablets, and computers. They should encourage their children to have outdoor exposure if just for one hour a day around the home like on the balcony, or garden. They should act as role models by reducing the time they spend on screen and spending more time with their children outdoors.
The use of digital devices for non-educational purposes should be reduced to less than 15 minutes per day for children using devices. Children should maintain at least an arm’s length working distance from the gadget, and make sure they work under good light. They should use large gadget screens for better resolution and increase font size for visual comfort. Children should frequently blink their eyes while on the system and also rest their eyes every 20 minutes for 20 seconds by looking at an object 20 feet away.
Conclusion:
According to the data obtained from this study, there has been no increase in the prevalence of myopia in the study population since the COVID-19 lockdown. However, the lifestyles of Nigerian children have since changed from the time of the lockdown and they now use more electronic devices for educational and recreational purposes. This reduces their outdoor activities and makes them spend more time on the screen. In the long term, there could be an increase in the incidence of myopia and its progression. Thus, the study’s recommendations should be endorsed.
Funding: Self-sponsored.
Acknowledgment: Not Applicable.
Conflicts of interest/Competing interest: Not Applicable.
Ethics approval: Lagos State University Teaching Hospital (LASUTH) Medical and Health Research Committee.
Consent to Participants: Signed by parents/guardians.
Consent for Publication: The manuscript has been read and approved by all the authors that the requirements for authorship as stated in this document have been met and each author believes that the manuscript represents honest work.